You are here
Peripheral Blood, systemic mastocytosis [LMP74199]
Keywords
Systemic mastocytosis, Cutaneous mastocytosis, mast cell, urticaria pigmentosa
Clinical History
A 24-year-old woman with recurring itchy skin, hives and flushing, difficulty swallowing and raspy voice with inspiratory stridor, cough and shortness of breath. She has had typical skin lesion of urticaria pigmentosa. There was no lymphadenopathy or organomegaly in physical examination.
Clinical Discussion
The accumulation of neoplastic populations of mast cells in the skin and other organs can lead to many different disease manifestations. The classic manifestation in the skin is urticaria pigmentosa (an itching rash and hyperpigmentation). The diagnosis of systemic mastocytosis is usually made by bone marrow biopsy.
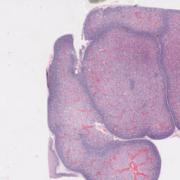
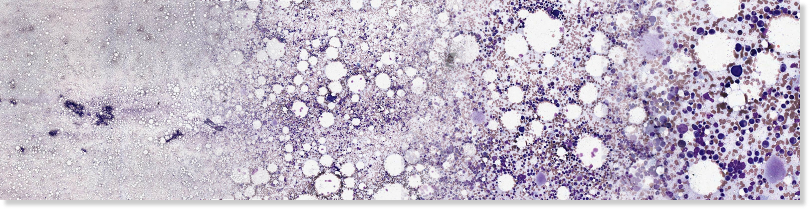
Morphologically, dense infiltrates of mast cells(>=15 mast cells in aggregates) are detected in a section of bone marrow and >25% of the mast cells in the infiltrate are spindle-shaped or have atypical morphology. In this case, the patient’s manifestations are relatively limited, consistent with an indolent subvariant of systemic mastocytosis.
Immunohistochemically, abnormal mast cells express CD2 and/or CD25 in addition to normal mast cell markers including tryptase, CD9,CD33,CD45, CD68 and CD117.
In this case the peripheral blood smear and bone marrow aspiration smear findings are unremarkable. The bone marrow biopsy shows aggregates of atypical mast cells. There are a few well-circumscribed non-paratrabecular lymphoid aggregates composed of a mixture of B and T-lymphocytes. Foci of moderate fibrosis are seen with a reticulin stain and they are associated with the mast cell and lymphoid aggregates. CD117 highlights scattered spindled mast cells which are also present in aggregates. The mast cells are positive for CD25 and mast cell tryptase and negative for CD2.
Flow cytometry of the bone marrow aspirate showed no evidence of a clonal B or T-cell population and 1% of the granulocyte population expressed mast cell markers CD117, CD25, CD34 and CD2. This correlates to the mast cell aggregates seen on the biopsy.
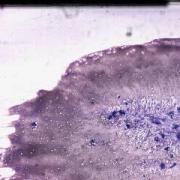
This slide shows peripheral blood smear, which was unremarkable. See Related Content for H&E, reticulin, CD25, CD117, tryptase, CD2, CD3 and CD20 stains of the bone marrow biopsy. Bone marrow aspiration smear (unremarkable) is also shown.
Morphologically, dense infiltrates of mast cells(>=15 mast cells in aggregates) are detected in a section of bone marrow and >25% of the mast cells in the infiltrate are spindle-shaped or have atypical morphology. In this case, the patient’s manifestations are relatively limited, consistent with an indolent subvariant of systemic mastocytosis.
Immunohistochemically, abnormal mast cells express CD2 and/or CD25 in addition to normal mast cell markers including tryptase, CD9,CD33,CD45, CD68 and CD117.
In this case the peripheral blood smear and bone marrow aspiration smear findings are unremarkable. The bone marrow biopsy shows aggregates of atypical mast cells. There are a few well-circumscribed non-paratrabecular lymphoid aggregates composed of a mixture of B and T-lymphocytes. Foci of moderate fibrosis are seen with a reticulin stain and they are associated with the mast cell and lymphoid aggregates. CD117 highlights scattered spindled mast cells which are also present in aggregates. The mast cells are positive for CD25 and mast cell tryptase and negative for CD2.
Flow cytometry of the bone marrow aspirate showed no evidence of a clonal B or T-cell population and 1% of the granulocyte population expressed mast cell markers CD117, CD25, CD34 and CD2. This correlates to the mast cell aggregates seen on the biopsy.
This slide shows peripheral blood smear, which was unremarkable. See Related Content for H&E, reticulin, CD25, CD117, tryptase, CD2, CD3 and CD20 stains of the bone marrow biopsy. Bone marrow aspiration smear (unremarkable) is also shown.
Related Content
Wholeslide Image ID: